Free Annual Physical Examination PDF Form
An annual physical examination is a cornerstone of preventive medicine and is crucial for maintaining good health and early detection of potential health issues. The comprehensive form designed for these examinations is meticulously structured to ensure that no aspect of a patient's health goes overlooked. At the outset, the form requires basic personal information, including name, date of birth, address, and Social Security Number, ensuring that the patient's medical records are accurately identified and stored. Further sections delve into detailed medical history, including diagnoses, significant health conditions, current medications, and any known allergies, which are pivotal for tailoring the examination and treatment to individual needs. Vaccination records and tuberculosis screening results are also recorded to assess the patient's immunization status and need for potential booster shots. The form extends its thoroughness to encompass tests like mammograms, prostate exams, and CBC/differential among others, reflecting a well-rounded approach to health screening. The general physical examination section meticulously assesses various systems of the body such as cardiovascular, respiratory, and nervous systems, to identify any abnormalities. Additionally, the form thoughtfully inquires about hospitalizations and surgical procedures to give the examining physician a complete medical history. Concluding with an evaluation and recommendations for health maintenance, including diet, exercise, and any necessary specialist consults, the form serves as a holistic tool for managing individual health care, ensuring that both patients and physicians are well-informed and prepared to address any health concerns proactively.
Sample - Annual Physical Examination Form
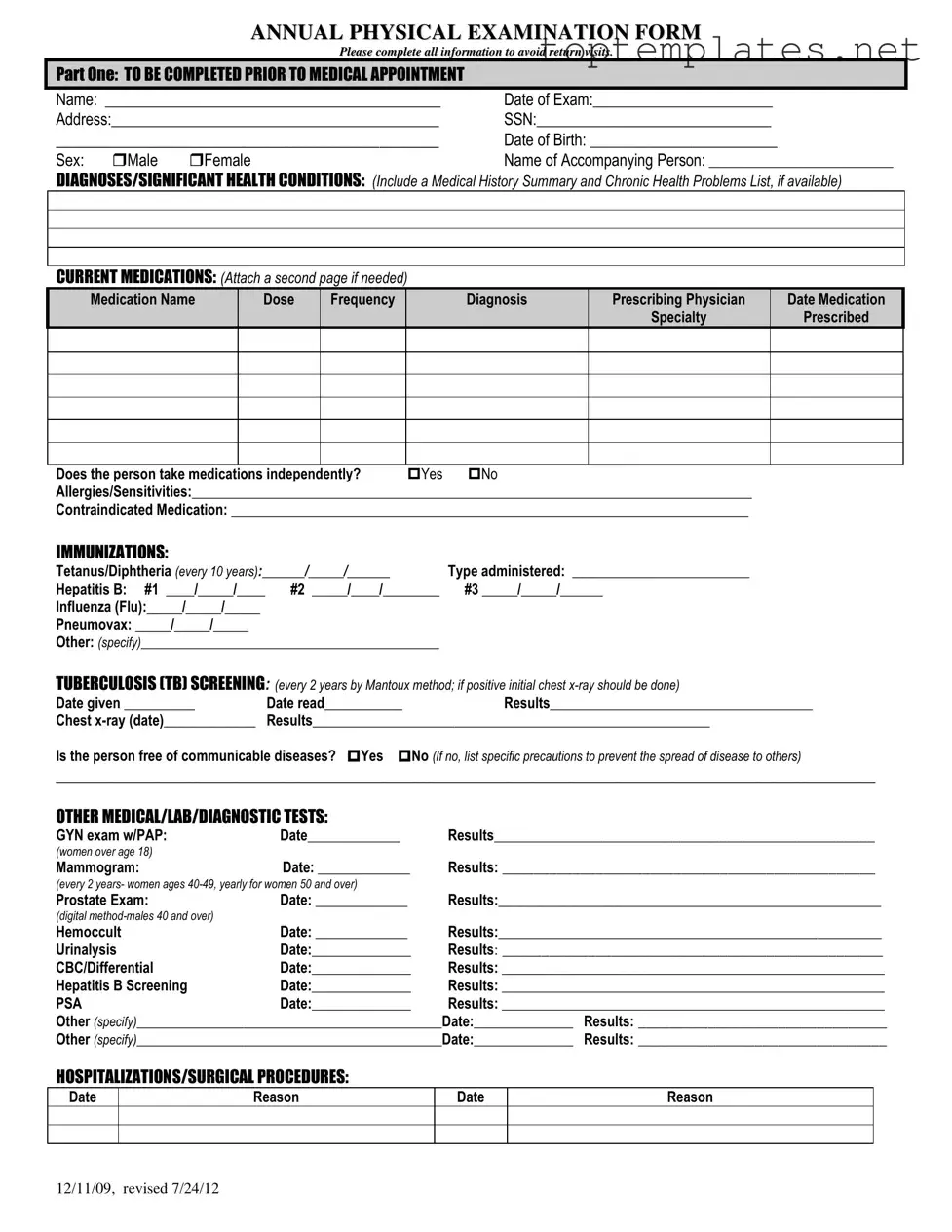
ANNUAL PHYSICAL EXAMINATION FORM
Please complete all information to avoid return visits.
PART ONE: TO BE COMPLETED PRIOR TO MEDICAL APPOINTMENT
Name: ___________________________________________ |
Date of Exam:_______________________ |
Address:__________________________________________ |
SSN:______________________________ |
_____________________________________________ |
Date of Birth: ________________________ |
||
Sex: |
Male |
Female |
Name of Accompanying Person: __________________________ |
DIAGNOSES/SIGNIFICANT HEALTH CONDITIONS: (Include a Medical History Summary and Chronic Health Problems List, if available)
CURRENT MEDICATIONS: (Attach a second page if needed)
Medication Name |
Dose |
Frequency |
Diagnosis |
Prescribing Physician |
Date Medication |
|
|
|
|
Specialty |
Prescribed |
Does the person take medications independently? |
Yes |
No |
Allergies/Sensitivities:_______________________________________________________________________________ |
||
Contraindicated Medication: _________________________________________________________________________
IMMUNIZATIONS:
Tetanus/Diphtheria (every 10 years):______/_____/______ |
Type administered: _________________________ |
|
Hepatitis B: #1 ____/_____/____ |
#2 _____/____/________ |
#3 _____/_____/______ |
Influenza (Flu):_____/_____/_____ |
|
|
Pneumovax: _____/_____/_____ |
|
|
Other: (specify)__________________________________________ |
|
|
TUBERCULOSIS (TB) SCREENING: (every 2 years by Mantoux method; if positive initial chest |
||
Date given __________ |
Date read___________ |
Results_____________________________________ |
Chest |
Results________________________________________________________ |
|
Is the person free of communicable diseases? Yes No (If no, list specific precautions to prevent the spread of disease to others)
_________________________________________________________________________________________________________
OTHER MEDICAL/LAB/DIAGNOSTIC TESTS:
GYN exam w/PAP: |
Date_____________ |
Results_________________________________________________ |
(women over age 18) |
|
|
Mammogram: |
Date: _____________ |
Results: ________________________________________________ |
(every 2 years- women ages
Prostate Exam: |
Date: _____________ |
Results:______________________________________________________ |
|
(digital |
|
|
|
Hemoccult |
Date: _____________ |
Results:______________________________________________________ |
|
Urinalysis |
Date:______________ |
Results: _________________________________________________ |
|
CBC/Differential |
Date:______________ |
Results: ______________________________________________________ |
|
Hepatitis B Screening |
Date:______________ |
Results: ______________________________________________________ |
|
PSA |
Date:______________ |
Results: ______________________________________________________ |
|
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
Other (specify)___________________________________________Date:______________ |
Results: ________________________________ |
||
HOSPITALIZATIONS/SURGICAL PROCEDURES:
Date
Reason
Date
Reason
12/11/09, revised 7/24/12

PART TWO: GENERAL PHYSICAL EXAMINATION
|
|
|
|
|
Please complete all information to avoid return visits. |
|
|
|
|
|
Blood Pressure:______ /_______ Pulse:_________ |
Respirations:_________ Temp:_________ Height:_________ |
Weight:_________ |
||||
|
|
EVALUATION OF SYSTEMS |
|
|
|
|
||
|
|
|
|
|
|
|
||
|
|
System Name |
|
Normal Findings? |
Comments/Description |
|
||
|
|
Eyes |
|
Yes |
No |
|
|
|
|
|
Ears |
|
Yes |
No |
|
|
|
|
|
Nose |
|
Yes |
No |
|
|
|
|
|
Mouth/Throat |
|
Yes |
No |
|
|
|
|
|
Head/Face/Neck |
|
Yes |
No |
|
|
|
|
|
Breasts |
|
Yes |
No |
|
|
|
|
|
Lungs |
|
Yes |
No |
|
|
|
|
|
Cardiovascular |
|
Yes |
No |
|
|
|
|
|
Extremities |
|
Yes |
No |
|
|
|
|
|
Abdomen |
|
Yes |
No |
|
|
|
|
|
Gastrointestinal |
|
Yes |
No |
|
|
|
|
|
Musculoskeletal |
|
Yes |
No |
|
|
|
|
|
Integumentary |
|
Yes |
No |
|
|
|
|
|
Renal/Urinary |
|
Yes |
No |
|
|
|
|
|
Reproductive |
|
Yes |
No |
|
|
|
|
|
Lymphatic |
|
Yes |
No |
|
|
|
|
|
Endocrine |
|
Yes |
No |
|
|
|
|
|
Nervous System |
|
Yes |
No |
|
|
|
|
|
VISION SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
HEARING SCREENING |
|
Yes |
No |
Is further evaluation recommended by specialist? |
Yes |
No |
|
|
ADDITIONAL COMMENTS: |
|
|
|
|
|
|
|
|
|
|
|
|
|
||
|
|
Medical history summary reviewed? |
Yes |
No |
|
|
||
Medication added, changed, or deleted: (from this appointment)__________________________________________________________
Special medication considerations or side effects: ________________________________________________________________
Recommendations for health maintenance: (include need for lab work at regular intervals, treatments, therapies, exercise, hygiene, weight control, etc.)
___________________________________________________________________________________________________________
Recommendations for manual breast exam or manual testicular exam: (include who will perform and frequency)____________________
___________________________________________________________________________________________________________
Recommended diet and special instructions: ____________________________________________________________________
Information pertinent to diagnosis and treatment in case of emergency:
___________________________________________________________________________________________________________
Limitations or restrictions for activities (including work day, lifting, standing, and bending): No Yes (specify)
___________________________________________________________________________________________________________ |
|||
Does this person use adaptive equipment? |
No |
Yes (specify):________________________________________________ |
|
Change in health status from previous year? No |
Yes (specify):_________________________________________________ |
||
This individual is recommended for ICF/ID level of care? (see attached explanation) Yes |
No |
||
Specialty consults recommended? No |
Yes (specify):_________________________________________________________ |
||
Seizure Disorder present? No Yes (specify type):__________________________________ Date of Last Seizure: ______________ |
|||
________________________________ |
_______________________________ |
_________________ |
|
Name of Physician (please print) |
Physician’s Signature |
|
Date |
Physician Address: _____________________________________________ |
Physician Phone Number: ____________________________ |
||
12/11/09, revised 7/24/12
File Specs
| Fact | Description |
|---|---|
| Completeness Requirement | All sections of the form must be completed to avoid the necessity for return visits. |
| Identification and History | Includes personal identification details, medical history summary, and a list of chronic health problems. |
| Medication and Allergies | Details about current medications, dosages, prescribing physician, allergies, and contraindicated medications are required. |
| Screenings and Exams | Documents screening and examination dates and results for a range of conditions and diseases, including recommendations for follow-up. |
Steps to Filling Out Annual Physical Examination
Filling out the Annual Physical Examination form is an essential step to ensure that a patient's medical records are up-to-date and comprehensive. This document plays a vital role in facilitating ongoing health maintenance and enables healthcare providers to tailor their care to the patient's specific needs. The process of completing this form can be straightforward if done meticulously, following each step carefully.
- Start by entering the patient's full name, the date of the examination, home address, Social Security Number (SSN), date of birth, and sex in the designated spaces in PART ONE.
- For the section named "Name of Accompanying Person," enter the name of the individual accompanying the patient to the medical appointment, if any.
- Under "DIAGNOSES/SIGNIFICANT HEALTH CONDITIONS", include any medical history summary, chronic health problems, and any current health issues. Attach additional pages if the space provided is insufficient.
- Detail the patient’s current medications, including the medication name, dose, frequency, diagnosis for which the medication was prescribed, prescribing physician, and specialty. If the patient takes medication independently, mark the appropriate box. Use an additional page if more space is needed.
- List all known allergies or sensitivities, along with any contraindicated medications, in the appropriate sections.
- Update the immunization records section with the most recent dates and types of vaccines administered, including those for Tetanus/Diphtheria, Hepatitis B, Influenza, Pneumovax, and any others specified.
- Provide the latest TB screening details, including the date it was given, read, and the results, along with any chest x-ray dates and outcomes. Mark whether the patient is free of communicable diseases and list specific precautions if needed.
- Record dates and results for additional medical, lab, or diagnostic tests, such as GYN exams with PAP smears, mammograms, prostate exams, and others requested.
- List any hospitalizations or surgical procedures with their dates and reasons.
- In PART TWO, fill in the general examination metrics, including blood pressure, pulse, respirations, temperature, height, and weight.
- Review and mark the evaluation of systems, checking "Yes" or "No" to indicate normal findings and provide comments or descriptions where necessary.
- Indicate the results of vision and hearing screenings and if further evaluation by a specialist is recommended.
- Make additional comments regarding the medical history summary, changes in medication, special considerations, health maintenance recommendations, dietary instructions, emergency treatment information, and any limitations or restrictions for activities.
- Update information on the use of adaptive equipment, changes in health status from the previous year, recommendations for specialty consults, and presence of seizure disorder, including the date of the last seizure.
- Complete the form with the printed name and signature of the physician, along with the date, physician's address, and phone number.
After successfully completing and reviewing the form for accuracy, it will be processed by the medical office. Following this, the patient may be advised on any further tests, treatments, or follow-ups required based on the comprehensive information provided in this document.
Discover More on Annual Physical Examination
What information is required when filling out the Annual Physical Examination form?
The Annual Physical Examination form necessitates comprehensive personal information, including the person's name, date of the exam, address, Social Security Number, date of birth, and sex. It also asks for the name of any accompanying person. Medical history, including diagnoses/significant health conditions, current medications, allergies, immunizations, TB screening results, and other medical/lab/diagnostic tests, must be detailed. Information on hospitalizations/surgical procedures, general physical examination findings, and additional comments regarding the health status, medication changes, and recommendations for health maintenance are also required.
Why is it important to complete all sections of the form?
Completing all sections of the form helps ensure a comprehensive evaluation of the person's health status. It prevents the need for return visits to provide missing information, which can delay necessary treatments or recommendations. Moreover, it enables healthcare providers to thoroughly understand the patient's medical history, current health conditions, and any potential risks, which is essential for delivering effective and personalized care.
What should be included in the diagnoses/significant health conditions section?
In the diagnoses/significant health conditions section, individuals should include a summary of their medical history and a list of chronic health problems. If available, attaching detailed documentation such as medical records or previous diagnosis reports can provide a thorough overview of the person's health condition, facilitating a more accurate and efficient assessment by the healthcare provider.
How should current medications be listed on the form?
Current medications must be listed with detailed information, including the medication name, dose, frequency of administration, diagnosis for which the medication is prescribed, prescribing physician's name, the specialty of the prescribing physician, and the date the medication was prescribed. If the person takes medications independently, this should also be indicated. If more space is needed, attaching a second page is recommended.
What are the requirements for the TB Screening and why is it important?
For Tuberculosis (TB) screening, the form specifies that it should be conducted every 2 years using the Mantoux method. If the initial test yields positive results, a chest x-ray should follow. This screening is vital for early detection of TB, preventing its spread to others, and facilitating prompt treatment. Indicating the dates of the test, reading, and results, along with any follow-up actions, is necessary.
How often should immunization information be updated?
Immunization information should reflect the most current status and be updated according to the vaccine's recommended schedule. For instance, Tetanus/Diphtheria boosters should be documented every 10 years, Hepatitis B series dates, Influenza annually, and other relevant vaccinations as administered. Accurate records ensure compliance with health recommendations and protect against preventable diseases.
What information is required for hospitalizations and surgical procedures?
For hospitalizations and surgical procedures, the form requests the dates and reasons for each event. Providing complete and accurate information about past hospital stays and surgeries helps healthcare providers understand the person's medical history in greater depth, including identifying any potential complications or recurrent health issues that may need ongoing management or observation.
Are there any specific instructions for the general physical examination section?
In the general physical examination section, readings for blood pressure, pulse, respirations, temperature, height, and weight should be entered. Additionally, evaluations of various systems (e.g., eyes, ears, nose, cardiovascular, musculoskeletal, etc.) require a notation of whether the findings were normal or not, with space for comments or descriptions. This information is crucial for catching any new or worsening health conditions early and adjusting care plans as necessary.
Common mistakes
When completing the Annual Physical Examination form, individuals often overlook or inaccurately provide crucial information, which can hinder the effectiveness of medical assessments and follow-ups. Addressing these common mistakes is vital for ensuring comprehensive healthcare. Here are six frequently observed errors:
Not filling in the Name or Date of Exam accurately: Omitting this basic yet essential information can delay the processing of the form and lead to potential mix-ups in medical records.
Leaving the SSN (Social Security Number) and Date of Birth fields blank: These identifiers are critical for distinguishing individual records and ensuring that the patient's medical history is accurately tracked.
Incompletely listing Diagnoses/Significant Health Conditions: Patients sometimes fail to mention all relevant health issues, which can impact the physician's ability to provide comprehensive care.
Omitting or incorrectly detailing Current Medications: This includes not providing the dosage, frequency, prescribing physician, or purpose of the medication, which is crucial for preventing drug interactions and managing health conditions.
Neglecting to update the Immunizations and Tuberculosis (TB) Screening sections: Accurate records of immunizations and TB screenings are important for public health and preventing the spread of communicable diseases.
Forgetting to mention any Allergies/Sensitivities or Contraindicated Medication: This information is vital in avoiding adverse reactions and ensuring the safety of medical treatments.
Avoiding these common mistakes not only improves the accuracy of the medical record but also enhances the quality of care a patient receives. Patients are encouraged to review their forms carefully and consult healthcare providers if there's any uncertainty in completing the form effectively.
Documents used along the form
The Annual Physical Examination form is integral in maintaining an individual's health record, providing a comprehensive overview of their current health status, including any significant health conditions, medications, and the results of various screenings and tests. Used in conjunction with other important medical forms and documents, it offers a fuller picture of the patient's health, facilitating better treatment and preventive care decisions. Below are nine other forms and documents frequently used alongside it:
- Medical History Summary: This document compiles past medical history, surgeries, hospitalizations, and family medical history, offering a broader context for understanding current health conditions.
- Medication List: A detailed record of all medications currently being taken by the patient, including dosage, frequency, and prescribing physician, it is crucial for monitoring medication management and avoiding drug interactions.
- Immunization Records: A log of all vaccinations received by the patient, this record helps ensure that the patient is up to date on all recommended vaccines, a key component in preventive health care.
- Consent Forms: These documents are signed by the patient or their guardian to consent to various medical treatments and procedures, providing legal protection and ensuring that patients are informed about their care.
- Insurance Information: Including insurance cards and forms, this documentation ensures that the medical services provided are within the network and coverage scope of the patient's insurance, facilitating billing processes.
- Advanced Directives: Legal documents specifying a patient's preferences for medical treatment if they become incapable of making decisions themselves, including living wills and durable power of attorney for health care.
- Screening Results: Documents detailing the findings of various medical screenings, such as mammograms, prostate exams, and colonoscopies, important for early disease detection.
- Laboratory Test Results: These include the results of blood tests, urine analysis, and other lab tests that provide critical data on the patient's health and are essential for diagnosing conditions.
- Referral Letters: Letters from a primary care physician referring the patient to specialists for further examination or treatment, indicating the reason for referral and pertinent patient health information.
Together, these documents and the Annual Physical Examination form create a complete health portfolio for the individual, guiding healthcare professionals in delivering effective care tailored to the patient's needs. Proper organization and maintenance of these documents are essential for achieving the best possible health outcomes.
Similar forms
Medical History Summary: Similar to the Annual Physical Examination form, a Medical History Summary gathers comprehensive health-related information from the patient. It includes past diagnoses, treatments, and surgeries, creating a historical health profile that medical professionals use to ensure accurate and holistic care. This parallel lies in the focus on collecting detailed health information to better understand and manage the patient's overall health.
Medication List: Just like the section on current medications in the Annual Physical Examination form, a Medication List documents all the medications a person is taking. This includes drug names, dosages, and frequency of intake. Its primary purpose is to inform healthcare providers about the patient's current medication regimen to prevent drug interactions and to consider these medications in the context of new diagnoses or treatments.
Immunization Record: This document lists all the vaccines an individual has received, similar to the immunizations section of the Annual Physical Examination form. The key aim is to track vaccine-preventable diseases and ensure that the individual is up-to-date with their immunizations, thereby promoting preventative healthcare practices.
Laboratory Test Results: Lab tests, such as blood work and urinalysis, are detailed in both the Annual Physical Examination form and standalone Laboratory Test Results documents. These results provide invaluable data on various parameters of the patient's health, such as glucose levels or kidney function, aiding in the diagnosis, monitoring, and treatment of conditions.
Tuberculosis (TB) Screening Record: The TB screening section of the Annual Physical Examination form is closely related to a standalone TB Screening Record, which verifies whether an individual has been screened for tuberculosis, the method used (e.g., Mantoux method), and the results. This screening is crucial for detecting TB and preventing its spread, underscoring the importance of maintaining up-to-date records for both individual and public health.
Surgical History Form: This form compiles a list of all surgical procedures a person has undergone, akin to the hospitalizations/surgical procedures section in the Annual Physical Examination form. It's essential for understanding a patient's past medical interventions, as surgical history can significantly influence current health status and future medical decision-making.
Health Maintenance Checklist: Similar to the recommendations for health maintenance section of the Annual Physical Examination form, a Health Maintenance Checklist is designed to track and prompt regular health screenings, tests, and treatments that are essential for preventing disease and maintaining overall health. It serves as a guide for both patients and healthcare providers to ensure that all aspects of health are actively managed.
Dos and Don'ts
Filling out an Annual Physical Examination form is crucial for ensuring you receive appropriate and timely medical care. Here's a guide to help you navigate the process smoothly:
What You Should Do:
- Be thorough and precise: Complete all sections of the form carefully, providing detailed information where necessary. If you're unsure about a question, it's better to seek clarification than to leave it unanswered.
- Review your medical history: Before filling out the form, gather any relevant medical records, lists of medications (including the dosage and frequency), and your immunization history. This helps ensure the information you provide is accurate and comprehensive.
- Update any changes in your health: If your health has changed since your last examination, make sure to include this information. This includes new diagnoses, changes in medication, or alterations in your health status.
- Prepare questions or concerns: If you have any health concerns or questions you want to discuss during your exam, jot them down beforehand. Include these notes with your form or keep them handy for your appointment.
- Check for completeness: After filling out the form, review it to ensure that you've answered every question and that your handwriting is legible. This can prevent unnecessary return visits or follow-up calls.
What You Shouldn't Do:
- Avoid leaving blanks: Don't skip sections or questions. If a question does not apply to you, it's better to write "N/A" (not applicable) rather than leaving it blank. This indicates to the healthcare provider that you didn't overlook the question.
- Don't guess: If you're uncertain about details such as dates of immunizations or specific diagnoses, don't guess. Instead, verify the information with your previous healthcare provider or check your medical records.
- Resist the temptation to underreport: Sometimes, there may be a temptation to leave out certain details about your health history or medication. However, withholding information can lead to incomplete care. Always be open and honest.
- Don't use medical jargon: Unless you're confident about its usage, avoid medical terminology. Misused terms can lead to misunderstandings. It's best to describe your health issues or concerns in clear, straightforward language.
- Avoid late submissions: Submitting your form well in advance of your appointment allows your healthcare provider time to review your information thoroughly. Late submissions can delay your exam and the delivery of appropriate care.
Misconceptions
When individuals approach their annual physical examination, a number of misconceptions can influence their expectations and perceptions about the process. By addressing these myths, we can ensure a better understanding and a more productive relationship with healthcare providers.
- Misconception 1: "Completing the form in advance is optional."
Many assume that filling out the form beforehand is merely a suggestion and not a requirement. However, providing detailed information prior to the appointment is crucial. It prevents delays, ensures more accurate care, and enables healthcare professionals to prepare for the visit effectively.
- Misconception 2: "The form doesn't need to include minor health issues."
There's a common belief that only significant health conditions should be reported. Yet, including all health concerns, even those perceived as minor, can give a more comprehensive health picture and impact care planning.
- Misconception 3: "All medications don't need to be listed, especially over-the-counter ones."
This overlooks the importance of understanding a person's complete medication regimen, including over-the-counter drugs, supplements, and prescribed medications. All can influence patient care and interact with each other in critical ways.
- Misconception 4: "Immunization history is irrelevant if I'm feeling fine."
Some might think their current health status makes immunization history unnecessary. However, updating and reviewing vaccination records can prevent future health issues and is a vital part of preventive care.
- Misconception 5: "The section on allergies and sensitivities is only concerning food."
It's often misunderstood that only food allergies matter. In reality, documenting all allergies, including medications, environmental factors, and materials, can be lifesaving by preventing adverse reactions during treatments or in emergency situations.
Dispelling these misconceptions is crucial for a well-informed and effective approach to annual physical exams. These examinations are a proactive measure for maintaining health, understanding potential risks, and establishing a trusted partnership with healthcare providers.
Key takeaways
When it comes to your health, being proactive and prepared can make a significant difference. The Annual Physical Examination form is an essential tool in this regard, helping you and your healthcare provider keep track of your health status and needs. Here are six key takeaways about filling out and using this form effectively:
- Complete All Sections Before Your Visit: To save time and ensure that your examination goes smoothly, fill out every part of the form before your appointment. This includes your personal information, medical history, current medications, allergies, immunizations, and any tests or screenings you've had.
- Update Your Medication List: Clearly list all the medications you're currently taking, including dosages, frequency, and the purpose of each medication. If necessary, attach an additional page. This helps prevent potential drug interactions and ensures your doctor can provide informed advice.
- Document Your Immunization History: Keep track of your immunizations, such as flu shots and tetanus vaccines. This information is crucial for maintaining up-to-date vaccinations and avoiding preventable diseases.
- Screening and Test Results: Include recent results from tests such as mammograms, cholesterol levels, blood pressure readings, or any other relevant screenings. These results offer vital insights into your health and can guide your healthcare provider in making accurate evaluations.
- Discuss Health Changes: Use the form to note any significant changes in your health since your last visit, including new diagnoses, hospitalizations, or alterations in your physical condition. This ensures your provider is fully aware of your current health status.
- Review and Update Annually: Health information changes over time. Reviewing and updating your Annual Physical Examination form each year before your check-up can help track your health trends and make informed decisions regarding your healthcare.
Filling out the Annual Physical Examination form with care and attention to detail can greatly enhance the effectiveness of your healthcare. It provides a comprehensive picture of your health, aids in disease prevention, and ensures you receive personalized care tailored to your needs.
Common PDF Forms
Pdf Free Printable Contractor Bid Forms - The document serves as an official record of the proposal, which can be useful for accounting and tax purposes for both the contractor and the client.
Form I-983 - For international students, the I-983 form is a step towards securing valuable U.S. work experience in their field of study, enhancing their employability post-graduation.
Faa Aircraft Bill of Sale - The AC 8050-2 serves as a definitive record of the sale, aiding in the resolution of any future disputes over aircraft ownership.