Valid Do Not Resuscitate Order Template
Decisions regarding end-of-life care are profoundly personal, yet they carry significant implications for the individual, their loved ones, and the healthcare professionals tasked with their care. Central to these decisions is the Do Not Resuscitate (DNR) Order form, a legal document that speaks on behalf of patients when they are no longer able to express their wishes about the use of CPR (cardiopulmonary resuscitation) in the event of cardiac or respiratory arrest. This form is not only a reflection of a person’s healthcare preferences but also an important piece of the broader conversation about patient autonomy and the ethics of medical intervention at the end of life. In navigating the complexities of this conversation, the DNR form serves as a critical tool, ensuring that the patient’s desires are known and respected by family members and healthcare providers alike. Understanding its role, the processes for its creation and implementation, and its impact on patient care requires a thoughtful exploration of both its legal and ethical dimensions. As such, the DNR form embodies the intersection of medical practice, law, and personal beliefs about death and dignity.
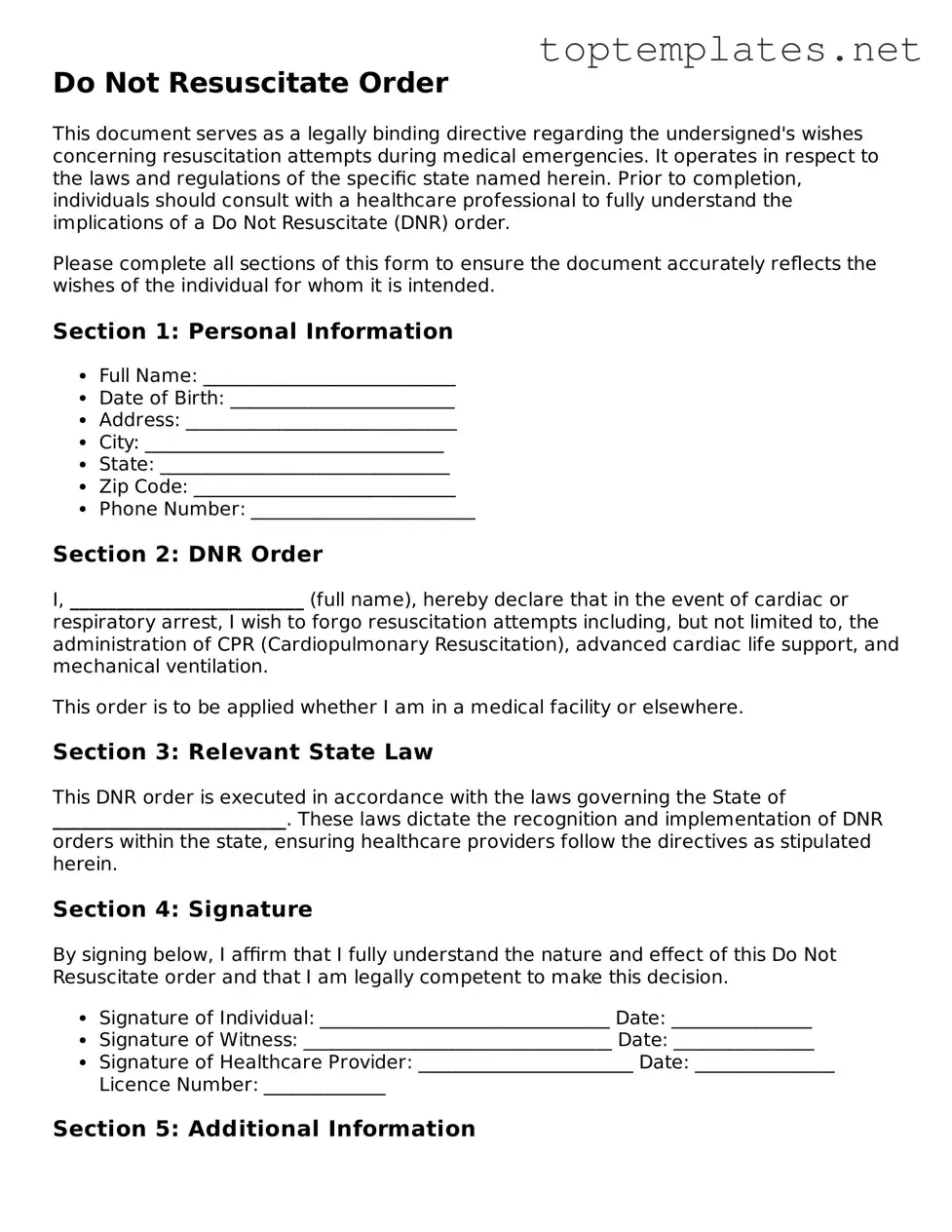
Sample - Do Not Resuscitate Order Form
Do Not Resuscitate Order
This document serves as a legally binding directive regarding the undersigned's wishes concerning resuscitation attempts during medical emergencies. It operates in respect to the laws and regulations of the specific state named herein. Prior to completion, individuals should consult with a healthcare professional to fully understand the implications of a Do Not Resuscitate (DNR) order.
Please complete all sections of this form to ensure the document accurately reflects the wishes of the individual for whom it is intended.
Section 1: Personal Information
- Full Name: ___________________________
- Date of Birth: ________________________
- Address: _____________________________
- City: ________________________________
- State: _______________________________
- Zip Code: ____________________________
- Phone Number: ________________________
Section 2: DNR Order
I, _________________________ (full name), hereby declare that in the event of cardiac or respiratory arrest, I wish to forgo resuscitation attempts including, but not limited to, the administration of CPR (Cardiopulmonary Resuscitation), advanced cardiac life support, and mechanical ventilation.
This order is to be applied whether I am in a medical facility or elsewhere.
Section 3: Relevant State Law
This DNR order is executed in accordance with the laws governing the State of _________________________. These laws dictate the recognition and implementation of DNR orders within the state, ensuring healthcare providers follow the directives as stipulated herein.
Section 4: Signature
By signing below, I affirm that I fully understand the nature and effect of this Do Not Resuscitate order and that I am legally competent to make this decision.
- Signature of Individual: _______________________________ Date: _______________
- Signature of Witness: _________________________________ Date: _______________
- Signature of Healthcare Provider: _______________________ Date: _______________ Licence Number: _____________
Section 5: Additional Information
For individuals under the care of a guardian, or if there are any durable power of attorney considerations, additional documentation may be required. These documents should be reviewed in conjunction with this DNR order to ensure all directives are harmonious and clearly understood by all parties involved.
It is recommended that copies of this DNR order be provided to the individual’s primary care physician, local hospital, and any relevant healthcare agencies to ensure the individual's wishes are known and can be readily accessed in an emergency.
File Breakdown
| Fact Name | Description |
|---|---|
| Purpose of DNR Orders | DNR (Do Not Resuscitate) Orders instruct medical professionals not to perform CPR (Cardiopulmonary Resuscitation) on patients whose breathing or heartbeat has stopped. |
| State-Specific Requirements | DNR form requirements and governing laws vary by state, affecting how the orders are issued, revoked, and recognized across state lines. |
| Issuance Process | Generally, a DNR order must be written by a healthcare provider based on the patient's wishes or those of the patient's legally designated healthcare proxy. |
| Impact on Medical Treatment | A DNR order does not affect other treatments. Patients with DNR orders still receive medical care aimed at comfort and the treatment of active health issues. |
| Revocation Process | Patients or their authorized representatives can revoke DNR orders at any time, necessitating clear communication with healthcare providers. |
Steps to Filling Out Do Not Resuscitate Order
Filling out a Do Not Resuscitate (DNR) Order is a crucial step for individuals wanting to express their wishes regarding the extent of medical interventions they receive, especially in life-threatening situations. This form allows a person to refuse certain life-sustaining treatments. It is important to carefully complete this form to ensure that your medical care preferences are clearly understood and respected by healthcare providers. The process involves several specific steps, starting with obtaining a form from the appropriate sources, usually healthcare providers or legal representatives.
- Obtain the Do Not Resuscitate Order form from your healthcare provider, legal representative, or download it from a verified state or healthcare institution's website.
- Read the instructions provided on the form carefully to ensure accurate completion and avoid any potential errors that could affect its validity.
- Enter the patient's full legal name, date of birth, and other identifying information as required on the form to ensure it is linked to the correct individual.
- If the form includes sections for specific medical conditions or scenarios in which the DNR order should apply, clearly indicate your choices as instructed. Be as specific as possible to prevent any ambiguity in emergency situations.
- Discuss your decision with a healthcare provider, as some states or institutions require a physician's signature to validate the DNR order. This discussion can also provide an opportunity to clarify any questions about the document's implications.
- Sign and date the form in the presence of any required witnesses or a notary, if applicable, according to your state's laws. This step often finalizes the document, making it legally binding.
- Submit a copy of the completed DNR order to your primary care physician and keep another copy in an easily accessible location at home. Inform family members or other caretakers of its existence and location.
- Consider wearing a DNR bracelet or carrying a wallet card that indicates you have a valid DNR order. This can help ensure that your wishes are followed even if you are outside of your home or in a setting where your primary documents are not immediately available.
After completing these steps, your Do Not Resuscitate Order will be effective. It’s recommended to review the document periodically, especially after any major health changes, to ensure that it continues to reflect your current wishes accurately. Adjustments can be made with the guidance of legal or healthcare professionals to keep the document up-to-date. Holding discussions with loved ones about your decision can also help family members understand and support your wishes, reducing potential conflicts or confusion in emergency situations.
Discover More on Do Not Resuscitate Order
What is a Do Not Resuscitate Order (DNR)?
A Do Not Resuscitate Order is a legal document signed by a patient and their healthcare provider. It instructs medical staff not to perform cardiopulmonary resuscitation (CPR) if the patient's breathing stops or if their heart stops beating.
Who can have a DNR order?
Any individual, regardless of their age or health condition, can choose to have a DNR order. However, it is typically considered by people with serious, life-limiting illnesses, or those who are near the end of life and prefer to pass away naturally without aggressive interventions.
How does one get a DNR order?
Obtaining a DNR order involves a conversation with your healthcare provider about your wishes regarding resuscitation and end-of-life care. If you decide a DNR order is right for you, both you and your healthcare provider must sign the DNR document to make it official.
Is the DNR order applicable in all healthcare settings?
DNR orders are generally respected across all healthcare settings, including hospitals, nursing homes, and in the home. However, it is essential to communicate your wishes and provide a copy of your DNR order to all healthcare providers and facilities involved in your care.
Can a DNR order be revoked or changed?
Yes. A DNR order is not permanent and can be revoked or changed at any time by the person to whom it applies. It's crucial to communicate any changes in your wishes to your healthcare provider, who can then help you update the DNR order.
Does having a DNR order affect the quality of other treatments?
No, having a DNR order does not affect the quality of treatment you receive for other medical conditions. It only provides specific instructions not to use CPR in the event your heart stops or you stop breathing. Your healthcare team will continue to provide all other appropriate treatments and care.
Are there any legal considerations or requirements for a DNR order to be valid?
While a DNR order is legally binding, requirements may vary from state to state. Typically, the DNR must be in writing, contain certain information, and be signed by both the patient (or their legally authorized representative) and the healthcare provider. It's important to consult with a healthcare provider or legal advisor to understand the specific requirements in your state.
Common mistakes
When filling out a Do Not Resuscitate (DNR) Order form, several common errors are made. These mistakes can significantly impact the efficacy of the directive and, by extension, the type of emergency care received. A DNR order is a critical document that specifies a person's desire not to have cardiopulmonary resuscitation (CPR) if their heart stops beating or if they stop breathing. Understanding and avoiding the following mistakes can ensure the person's wishes are clearly communicated and respected during emergencies.
Not Consulting with Healthcare Providers: Many individuals complete the DNR form without seeking advice from their healthcare providers. This oversight can result in misunderstandings about the medical implications of a DNR order and how it fits into the broader context of the individual's overall healthcare plan. It's crucial for individuals to discuss their wishes and understand the medical facts from professionals before making such a significant decision.
Incomplete or Incorrect Information: The form must be filled out accurately and completely. Missing information or errors in personal details, such as the individual's full name, date of birth, or specific medical information, can invalidate the order or cause confusion among healthcare providers. It's essential to review the form thoroughly and ensure all information is correct and legible.
Failure to Update the Form: Healthcare wishes and needs can evolve over time. A DNR order made years ago may no longer reflect an individual's current wishes. However, many fail to review and update their DNR orders regularly. It's advisable to revisit this document periodically, especially after any significant health changes, to ensure it still represents the individual's desires accurately.
Lack of Proper Witnesses or Notarization: Depending on state laws, a DNR order may need to be witnessed or notarized to be considered valid. Not adhering to these legal requirements can render the document ineffective. Individuals should familiarize themselves with their state's specific requirements and ensure their DNR order complies with these regulations.
By being mindful of these common pitfalls when completing a Do Not Resuscitate Order form, individuals can better guarantee that their healthcare wishes will be respected and followed during critical moments. It's a document that demands careful consideration, precise information, and regular updates to mirror one’s current health care preferences accurately.
Documents used along the form
While the Do Not Resuscitate (DNR) Order form is crucial for those who wish to decline resuscitation in the case of respiratory or cardiac arrest, it is often just one part of a broader collection of documents aimed at guiding medical care according to an individual's wishes. Understanding these documents can help individuals and their families ensure that their healthcare preferences are respected and followed.
- Living Will - This document allows individuals to outline their preferences for medical treatment in various scenarios should they become unable to communicate their wishes. It often includes directions regarding the use of life-sustaining measures in the case of terminal illness, irreversible coma, or severe brain damage.
- Health Care Power of Attorney (HCPOA) - The HCPOA enables an individual to appoint someone they trust to make healthcare decisions on their behalf if they're unable to do so. This document is critical in ensuring that the chosen representative understands the individual's preferences, including their wishes about DNR orders.
- Physician Orders for Life-Sustaining Treatment (POLST) - The POLST form complements a DNR by providing specific instructions regarding other types of life-sustaining treatments, such as feeding tubes or ventilator use. It's particularly useful for those with serious illnesses, as it is designed to travel with the patient across different care settings.
- Medical Orders for Scope of Treatment (MOST) - Similar to the POLST, the MOST form provides detailed wishes concerning the extent of medical treatments an individual desires. It is especially beneficial in clarifying which life-sustaining treatments, if any, a person wants to receive beyond just resuscitation.
- Advance Directive - Often encompassing aspects of the living will and the HCPOA, an advance directive is a broader document that specifies an individual's healthcare preferences, including end-of-life care and the appointment of a healthcare proxy. It's a foundational element in planning for healthcare needs.
Incorporating these documents into one's healthcare plan can significantly affect the care received during critical moments. By clearly stating one’s medical treatment preferences, individuals can provide a clear guide for family members and healthcare providers, helping to reduce stress during emergency situations and ensuring that their healthcare wishes are known and respected.
Similar forms
Living Will: Like a Do Not Resuscitate (DNR) order, a living will specifies an individual's healthcare preferences, particularly concerning end-of-life care. It provides instructions on the use of life-sustaining treatments or procedures when a person is unable to communicate their wishes due to a medical condition.
Healthcare Power of Attorney: This document appoints someone to make healthcare decisions on an individual’s behalf when they are incapacitated. It's similar to a DNR in that it concerns decisions about medical care, though it covers a broader range of decisions beyond resuscitation.
Advance Directive: An advance directive encompasses a living will and can also include a DNR order and the designation of a healthcare proxy or power of attorney. It's a more comprehensive document regarding future healthcare preferences, including but not limited to resuscitation wishes.
POLST (Physician Orders for Life-Sustaining Treatment): Similar to a DNR, a POLST provides specific instructions about life-sustaining treatment preferences in the form of medical orders. Whereas a DNR specifically addresses the absence of CPR, a POLST can cover a range of treatments, such as the use of ventilators, antibiotics, and artificial nutrition and hydration.
Five Wishes Document: This patient-friendly form acts like an advance directive that addresses personal, emotional, and spiritual needs as well as medical wishes. It goes beyond a DNR by including a person’s desires about their comfort, how they want to be treated, and what they want their loved ones to know.
Medical Orders for Scope of Treatment (MOST): Similar to POLST, MOST is designed for individuals facing a serious illness and outlines a comprehensive plan for end-of-life care, including resuscitation preferences. It's specifically aimed at ensuring that a patient's treatment preferences are followed across settings.
Last Will and Testament: While primarily used for dictating the distribution of assets and guardianship wishes, a Last Will and Testament can also include personal statements about an individual's desires for funeral arrangements or memorials. It’s similar in the aspect of preparing for end-of-life issues, though it does not directly address medical treatment preferences like a DNR.
Dos and Don'ts
When it comes to completing a Do Not Resuscitate (DNR) Order form, it's essential to approach the task with diligence and care. The document is a critical part of a person's healthcare directive, ensuring their wishes are respected during emergency situations. Below are several dos and don'ts to consider:
Do:
- Consult with a healthcare provider: Before filling out the form, it’s important to discuss your wishes and any medical questions you might have with a healthcare professional.
- Use clear, precise language: Ensure that all instructions are written clearly to avoid any possible confusion during emergency situations.
- Verify state requirements: Since laws can vary by state, verify that the form meets all local legal requirements and includes any specific state mandates.
- Include relevant medical information: Provide any necessary medical history or information that might be relevant to the DNR order.
- Sign and date the form: Make sure the form is signed and dated correctly, as this is often a legal requirement for the document to be valid.
- Make copies: After the form is completed, make several copies. Keep one for yourself and distribute others to your healthcare proxy, family members, and primary physician.
- Review periodically: Circumstances and wishes can change. Review and, if necessary, update your DNR order regularly to ensure it still reflects your current wishes.
Don't:
- Fill out the form alone: While you can fill out the form by yourself, it's recommended to do it with the assistance of a healthcare provider or legal professional to ensure all aspects are covered accurately.
- Use ambiguous language: Avoid using terms or phrases that could be interpreted in more than one way to prevent any confusion during critical moments.
- Forget to communicate your wishes: After completing the form, have a conversation with family members and your healthcare proxy about your decisions to ensure everyone is informed.
- Overlook local laws: Failing to adhere to state-specific requirements can result in a DNR order being considered invalid.
- Leave fields incomplete: Ensure no sections are left blank unless specified, as incomplete information might question the validity of the document.
- Fail to notify your medical providers: Inform your entire healthcare team about your DNR order, especially if any changes are made.
- Ignore reviewing the document: Regularly review the DNR order to make certain it reflects your most up-to-date wishes, especially after any major health diagnosis or change in thinking.
Misconceptions
When it comes to end-of-life care, a Do Not Resuscitate (DNR) order is one of the most misunderstood medical documents. Although it plays a crucial role in the medical care of an individual, several misconceptions persist about its use and implications. Understanding these misconceptions can help patients and their families make informed decisions regarding end-of-life care. Below are five commonly misunderstood aspects of the DNR order.
- DNR orders are only for the elderly. A common belief is that DNR orders are exclusively for older patients. However, these orders are applicable to any patient, regardless of age, who does not wish to have cardiopulmonary resuscitation (CPR) in the event their heart stops or they stop breathing. This decision is based on individual health situations and personal values, not just age.
- A DNR means no medical treatment will be provided. Another misconception is that a DNR order means the patient will not receive any medical treatment. In reality, a DNR order specifically refers to the non-performance of CPR in the event of cardiac or respiratory arrest. Patients with a DNR order still receive all other appropriate treatments and palliative care aimed at comfort and management of symptoms.
- DNR orders are permanent and cannot be changed. It's often thought that once a DNR order is made, it cannot be altered. This is not accurate; a DNR order can be revoked or modified at any time by the patient or their legally authorized representative. Medical wishes and preferences can change, and so too can DNR orders, to reflect these changes.
- Only a physician can initiate a DNR order. While it is true that a DNR order must be signed by a physician to be medically binding, the initiation of the conversation can come from patients or their designated healthcare proxies. Individuals have the right to discuss and express their wishes regarding CPR with their healthcare providers.
- A DNR order applies in all situations. Some people believe that a DNR order is applicable in every medical scenario. However, DNR orders typically apply to situations where cardiac or respiratory failure occurs. They do not apply to other medical interventions unless specifically stated. Furthermore, DNR orders made in a hospital setting might not automatically transfer to other settings like home or hospice care; this requires separate documentation.
Key takeaways
The Do Not Resuscitate (DNR) Order form is a critical document for individuals who wish to express their preferences regarding life-saving treatments. Below are key takeaways regarding the completion and utilization of a DNR form.
- A DNR order must be completed in consultation with a healthcare provider. This ensures that the individual understands the implications of the order.
- The form should be fully completed to ensure it is legally valid. Missing information can lead to confusion or misinterpretation in emergency situations.
- Discussing end-of-life wishes with family members and loved ones is important before completing a DNR order. This can help avoid conflicts or surprises during critical moments.
- The DNR order needs to be easily accessible and visible for emergency personnel. Some people opt to keep it on their refrigerator or in an easily seen location.
- Carrying a wallet card or wearing a bracelet indicating the existence of a DNR order can also be critical in ensuring the order is followed outside the home.
- Health conditions of an individual can change over time. It’s necessary to review and possibly update the DNR order periodically.
- Every state has its own specific form and regulations regarding DNR orders. It’s crucial to use the correct form for your state to ensure it is binding.
- DNR orders are specific to cardiopulmonary resuscitation (CPR). They do not apply to other medical interventions. Other documents, such as a living will, may be required to address broader medical wishes.
- In some states, DNR orders can also be included in an electronic registry to ensure accessibility by healthcare providers.
- If an individual decides to revoke their DNR order, it’s essential to inform all relevant parties, including healthcare providers and family members, to avoid any confusion.
Consider Other Documents
Boyfriend Application Form - Although informal, the Boyfriend Application Form prompts individuals to consider what they are truly seeking in a relationship, aiding in self-awareness and clarity.
Cg2010 Form - The endorsement outlines that any insurance coverage extended to additional insureds is confined by law and will not exceed the scope of coverage mandated by any contract or agreement requiring their addition.