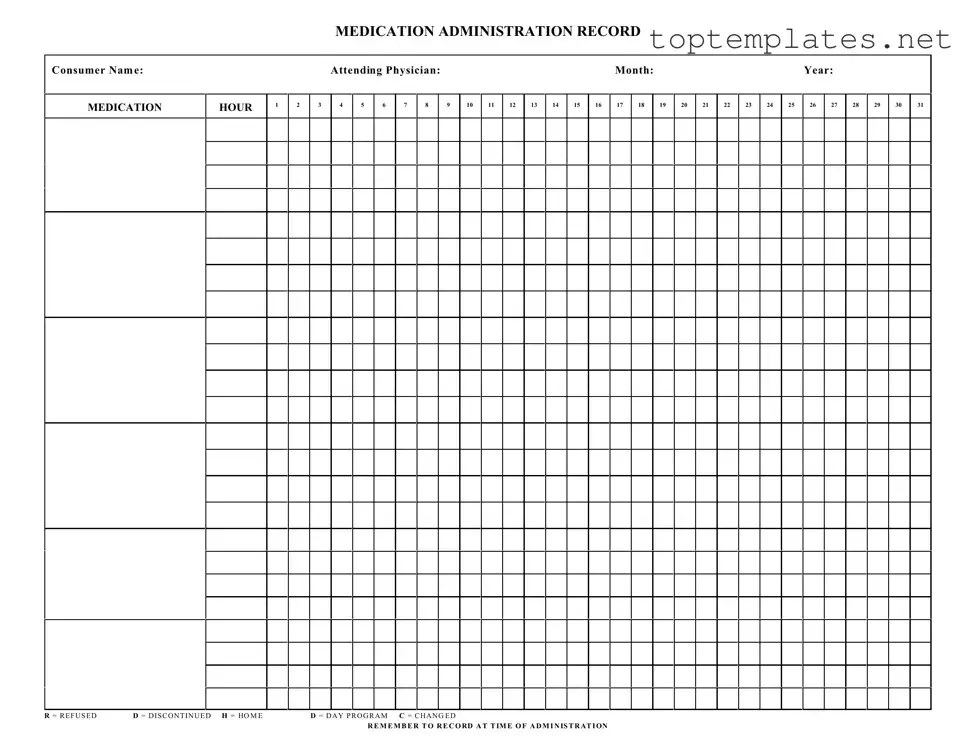
Free Medication Administration Record Sheet PDF Form
The Medication Administration Record Sheet is a vital document in the healthcare and caregiving industries, designed to ensure the accurate administration of medications to consumers. This detailed form includes essential information such as the consumer's name, the attending physician, and specific medication hours throughout the month, providing a comprehensive timeline for medication administration. Significantly, the form includes codes such as 'R' for refused, 'D' for discontinued, 'H' for home, 'D' for day program, and 'C' for changed, which are crucial for recording any deviations from the prescribed regimen. Healthcare professionals are reminded to fill out this form at the time of medication administration, emphasizing the importance of accuracy and timeliness in medication management. This process not only aids in maintaining an organized record for individual care but also supports regulatory compliance and ensures the well-being of the consumers under care.
Sample - Medication Administration Record Sheet Form
MEDICATION ADMINISTRATION RECORD
Consumer Nam e:
MEDICATION
HOUR
1
2
|
Attending Physician: |
|
|
|
|
|
|
|
|
Month: |
|
|
|
|
|
|
|
Year: |
|
|
|
|
||||||||
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
3 |
4 |
5 |
6 |
7 |
8 |
|
9 |
10 |
11 |
12 |
13 |
14 |
15 |
16 |
17 |
18 |
|
19 |
20 |
21 |
22 |
23 |
24 |
25 |
26 |
27 |
28 |
29 |
30 |
31 |
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
|
R = R E F U S E D |
D = D I S C O N T I N U E D H = HO M E |
D = D A Y P R O G R A M C = C H A N G E D |
R E M E M B E R T O R E C O RD A T T IM E O F A D M I N IS T R AT I ON
File Specs
| Fact Name | Description |
|---|---|
| Primary Purpose | Used to accurately record the administration of medications to a consumer over a period of time. |
| User | Typically utilized by healthcare providers, including nursing staff and caregivers in various settings. |
| Key Elements | Includes consumer name, medication, hour of administration, attending physician, and dates of the month. |
| Special Codes | Features codes such as "R" for refused, "D" for discontinued, "H" for home, "D" for day program (appears to be duplicated), and "C" for changed. |
| Recording Time | Medical professionals are reminded to record the time of medication administration as it occurs. |
| Frequency of Use | This form is updated daily to ensure all medication administrations are documented in real-time. |
| Legal Importance | Maintaining an accurate Medication Administration Record (MAR) is crucial for legal, medical, and billing accuracy purposes. |
| Governing Laws | Varies by state; however, generally regulated under state health and nursing laws concerning medication management and administration. |
| Version Control | It is important to use the most current version of the form to comply with updated health regulations and practices. |
Steps to Filling Out Medication Administration Record Sheet
Filling out a Medication Administration Record (MAR) Sheet accurately is imperative for ensuring that individuals receive their medications correctly and at the right times. The MAR Sheet is a comprehensive tool used to document all medication administered throughout the month, making it an essential record for healthcare providers, caregivers, and individuals receiving care. Each section of the form has a specific purpose, from indicating the consumer's name and attending physician to detailing each medication's administration hour by hour, day by day throughout the month. Here's how to properly fill out the form:
- Consumer Name: Enter the full name of the individual receiving the medication to ensure the record is accurately attributed.
- Attending Physician: Write down the name of the physician who prescribed the medications to link the prescriptions back to the healthcare provider for any necessary follow-up.
- Month and Year: Clearly state the month and year to which the medication administration record applies, providing a temporal context for the record.
- Under the MEDICATION HOUR section, which is labeled from 1 to 31 to correspond with the days of the month, note the specific times medications are to be administered. Each hour has a dedicated space; utilize this area to keep accurate timing records.
- When a medication is administered, record the event by marking the appropriate box under the day it was given. Ensure accuracy to maintain a reliable administration schedule.
- If the consumer refuses medication, mark the box with an "R" for REFUSED. This information is critical for healthcare providers to assess and address any issues with medication compliance.
- Should a medication be discontinued, indicate this change by entering a "D" for DISCONTINUED on the corresponding day and hour. This helps maintain an up-to-date medication schedule.
- When documenting a change in medication or its administration, use "C" for CHANGED. This ensures that all medication adjustments are promptly and accurately recorded.
- If the consumer is attending a day program or is at home when the medication is administered, mark the corresponding "H" for HOME or "D" for DAY PROGRAM to note the location of administration. This detail provides context relevant to the individual’s daily routine and care environment.
- Lastly, remember to document each administration at the time it occurs. Timely record-keeping prevents discrepancies and ensures the Medication Administration Record Sheet accurately reflects the individual's medication management.
Filling out the Medication Administration Record Sheet with precision is a critical task in managing an individual's healthcare regime. By following these steps, caregivers and healthcare providers can ensure that medication administration is accurately tracked, supporting effective and safe care practices.
Discover More on Medication Administration Record Sheet
What is a Medication Administration Record Sheet?
A Medication Administration Record Sheet, often referred to as a MAR, is a comprehensive chart used in healthcare settings to record all the medications prescribed and administered to a patient over a certain period. This document includes critical information such as the consumer’s name, medication details, dosage times, attending physician, and the specific month and year of the record. It also provides a system for noting any changes to the medication regimen, including refused, discontinued, or altered doses.
How is the "R = REFUSED D = DISCONTINUED H = HOME D = DAY PROGRAM C = CHANGED" notation used?
This notation system allows healthcare providers to quickly document the status of each medication dose. If a patient refuses a dose, "R" is marked; if the medication is discontinued, "D" is noted; a dose taken at home is marked as "H"; "D" can also stand for medications taken while in a day program, and "C" indicates any change in the medication regimen. This efficient method ensures clarity and accuracy in the patient’s medication administration record.
Why is it important to record medication at the time of administration?
Recording medication at the time of administration is crucial for maintaining an accurate and up-to-date account of a patient's medication management. This practice minimizes the risk of errors, such as double dosing or skipping a dose, thus ensuring the patient receives the proper care. Furthermore, it supports accountability and provides a clear audit trail that can be essential in evaluating the patient's response to treatment and making informed healthcare decisions.
What should you do if a patient refuses medication?
If a patient refuses medication, it is important to record the refusal in the MAR using the "R" notation and immediately notify the attending physician or a healthcare provider. Understanding and documenting the reason for refusal can be valuable for assessing whether adjustments to the treatment plan are necessary. It’s also essential to ensure that the patient is informed about the potential risks of skipping their medication.
How does the MAR handle changes in medication?
Changes in a patient's medication regimen are common and are handled meticulously in the MAR. When a medication is changed—whether in dosage, time, or even when discontinuing it—this alteration is noted with a "C" for changes or "D" for discontinued. Recording these changes diligently ensures that all healthcare providers involved in the patient's care are up-to-date with the most current treatment plan.
What is the significance of noting medications taken at home or in a day program?
The notations "H" for home and "D" for day program are significant because they acknowledge the different environments in which a patient may receive medication. This distinction is essential for coordinating care and ensuring continuity. It helps healthcare providers understand the full scope of the patient’s medication regimen, including doses administered outside of the primary healthcare setting, leading to a more comprehensive approach to treatment and monitoring.
Common mistakes
When handling a Medication Administration Record Sheet (MAR), accuracy and attention to detail are crucial. Several common errors can compromise the effectiveness of the document, impacting patient care. Here are nine mistakes to avoid:
Failing to double-check the consumer's name against the medication orders to ensure accuracy can lead to administering medication to the wrong individual.
Omitting or inaccurately recording the attending physician's name may create confusion or delay should clarification on the medication order be necessary.
Not specifying the month and year at the top of the form can result in using outdated or incorrect medication orders.
Incorrectly marking the medication hour or failing to record the time of administration accurately may result in administering medication at the wrong time.
Overlooking the key for R (Refused), D (Discontinued), H (Home), and C (Changed) can lead to misinterpretation of the patient's medication history.
Forgetting to mark or incorrectly marking a medication as refused, discontinued, taken at home, or changed can lead to potential health risks or medication errors.
Not recording the administration of medication precisely at the time it occurs can contribute to errors in medication timing and frequency.
Misunderstanding or not using the provided key (R, D, H, C) correctly could lead to incorrect assumptions about medication administration or changes.
Neglecting to review and verify the accuracy of each entry before concluding can allow errors to go unnoticed and uncorrected.
To prevent these common errors:
Always verify the consumer's details and the month and year on the MAR against current records.
Ensure that medication times are accurately recorded, and consult the attending physician or pharmacist if any uncertainties arise.
Utilize the key provided (R, D, H, C) consistently to denote medication status, and make sure to document any medication that is refused, discontinued, taken at home, or changed.
Regularly review the MAR for accuracy, and correct any discrepancies as soon as they are noticed.
By avoiding these mistakes, healthcare providers can ensure that the Medication Administration Record Sheet is an accurate and effective tool for documenting and managing patient care.
Documents used along the form
When navigating the healthcare system, especially for those under long-term care, managing and administering medication requires meticulous attention to detail. The Medication Administration Record (MAR) Sheet is a cornerstone document in ensuring that medications are given correctly and at the right times. However, for a comprehensive view of a patient's care, the MAR Sheet is often used in conjunction with several other forms and documents. Each plays a vital role in delivering care, managing treatments, and ensuring patient safety.
- Physician's Orders: This document outlines the specific instructions given by a doctor or a medical professional regarding a patient's care, including medications, doses, and administration methods. It provides the legal and medical foundation for the MAR Sheet.
- Individual Service Plan (ISP): The ISP is tailored for patients requiring long-term care, detailing personalized goals and interventions, including medication management, to ensure comprehensive care is provided.
- Consent Forms: These are necessary for acknowledging and documenting the patient or guardian's consent to receive the medications listed on the MAR Sheet, including any potential risks or side effects.
- Medication Reconciliation Form: Used to compare a patient’s medication orders to all of the medications that the patient has been taking. This form helps to avoid duplication, omissions, dosing errors, or drug interactions.
- Allergy Documentation: This critical form records any known allergies a patient has, particularly to medications, ensuring that these are cross-referenced before administration.
- Incident Report Forms: In the event of an adverse reaction or medication error, incident reports provide a structured way to document what happened, including any steps taken after the incident.
- Treatment Administration Records (TAR): Similar to the MAR, the TAR tracks non-medication treatments administered to the patient, ensuring a holistic overview of care.
- Drug Disposal Forms: For tracking the disposal of unused, discontinued, or expired medications, ensuring compliance with regulations and reducing the risk of misuse.
- Nursing or Caregiver Notes: These notes offer insights into the patient's response to medications, side effects, or any observations that might indicate a need to adjust treatment. They form a narrative supplement to the more structured MAR Sheet.
Together, these documents create a comprehensive ecosystem of care documentation essential for safely administering medication and managing a patient's healthcare. They ensure that every aspect of medication administration is documented, communicated, and acted upon properly, reflecting an integrated approach to patient care. Comprehensive documentation not only supports the delivery of high-quality healthcare but also enhances communication among different care providers, thereby improving outcomes for patients under long-term care.
Similar forms
Patient Progress Notes: Similar to the Medication Administration Record Sheet, Patient Progress Notes are used by healthcare professionals to document the care and treatment of patients over time. Both forms are integral in tracking the patient's healthcare journey, including any changes in medication or treatment plans.
Daily Nursing Flow Sheet: Nurses use this document to record vital signs, treatments, and care provided to the patient throughout their shift, much like how the Medication Administration Record tracks medication dosages and times. Both sheets ensure continuity of care and communication among healthcare staff.
Patient Treatment Plan: This document outlines a patient's overall treatment strategy, including medications, therapies, and goals, similar to how the Medication Administration Record outlines the medication regimen. Both are crucial for coordinating and managing a patient's healthcare.
Prescription Pad Sheets: Written by physicians, these sheets authorize the dispensing of medications to patients. They are similar in function to the Medication Administration Record, which tracks the administration of those prescribed medications.
Medical Orders Sheet: This document details specific instructions from doctors regarding a patient's care, including medication orders. It is closely related to the Medication Administration Record Sheet, serving as a basis for the medications listed on the MAR.
Pharmacy Prescription Dispensing Log: Pharmacies use logs to track the dispensing of medications to patients. These logs complement the information found on a Medication Administration Record, providing a full view of a patient’s medication history.
Immunization Record: Although focusing specifically on vaccinations, Immunization Records track a patient's vaccine history over time, akin to how a Medication Administration Record tracks medication administration. Both are essential for understanding a patient's medical history.
Dietary Order Forms: Used in healthcare settings to document and communicate patient dietary needs and restrictions, these forms share a similar goal with the Medication Administration Record of ensuring that the patient's health care plans, including nutritional needs, are followed accurately.
Anesthesia Record: Anesthesia records document all anesthesia administered during surgery, including times and dosages, similar to the Medication Administration Record's tracking of medication administration. Both are critical for patient safety and care continuity.
Emergency Room (ER) Treatment Record: This document logs all treatments and medications administered during a patient's visit to the ER, offering a comprehensive overview of the care provided, paralleling the Medication Administration Record's role in chronicling medication administration.
Dos and Don'ts
When filling out the Medication Administration Record Sheet, several practices should be followed to ensure the accuracy and legality of the document. Below is a list of things you should and shouldn't do:
Do:
- Verify the consumer's information : Double-check the name, attending physician, month, and year fields to ensure they are correct.
- Record at the time of administration : To maintain accuracy, note the medication's administration as it happens.
- Use clear and legible handwriting : To ensure that anyone who reads the form can understand the entries, write neatly and clearly.
- Mark the correct box accurately: For each medication administered, carefully mark the corresponding hour accurately.
- Document any changes : If there's any alteration in the medication regime, note it on the form along with the date and reason for change.
- Indicate refusals properly : If a consumer refuses medication, mark "R" in the relevant box and provide details if necessary.
- Sign each entry : After administering medication or noting an observation, sign your initials to verify the action taken.
Don't:
- Guess information : If you’re unsure about any details, verify them before making an entry.
- Overwrite errors : Instead of trying to correct errors by overwriting, strike through mistakes clearly and enter the correct information next to it, then initial the correction.
- Leave blanks : If a medication was not administered, indicate the reason rather than leaving blank spaces.
- Use jargon or abbreviations not approved by your facility: Stick to known and approved abbreviations to avoid confusion.
- Forget to record details of refused, discontinued, or changed medications : Be detailed in your notations to ensure clarity for anyone reviewing the form.
- Postpone documentation : Delaying to fill out the form can lead to inaccuracies or forgotten details.
- Ignore confidentiality protocols : Always maintain the privacy of consumer information according to your facility's standards and legal requirements.
Misconceptions
There are several misconceptions about the Medication Administration Record (MAR) Sheet form that can affect both the quality of care provided to patients and compliance with healthcare regulations. Understanding these misconceptions is crucial for caregivers, medical personnel, and patients alike.
-
Misconception 1: MAR Sheets Are Primarily for Doctors and Nurses Only
While it's true that healthcare professionals use MAR sheets to ensure proper medication administration, it's also important for caregivers and patients, especially in long-term care or home care settings. Everyone involved in the medication administration process should understand how to read and update the MAR sheet to maintain accurate records. -
Misconception 2: Digital MAR Sheets are Prone to More Errors than Paper MAR Sheets
This is not necessarily true. Digital MAR sheets can reduce the likelihood of manual errors, provide automatic updates, and ensure better legibility. The key is proper training and adherence to protocols when using digital systems. -
Misconception 3: Once Medication is Discontinued, It Should Be Removed from the MAR Sheet
While discontinued medications are no longer administered, their record should remain on the MAR sheet for a period. This practice ensures there is a comprehensive medication history for each patient, which is crucial for understanding past treatment regimens and outcomes. -
Misconception 4: All Errors on a MAR Sheet Can Result in Legal Liability
Errors in medication administration are serious, but not all errors result in liability. The key factors are the nature of the error, the harm caused, and the actions taken once the error was discovered. Properly documenting and addressing errors can mitigate potential legal issues. -
Misconception 5: MAR Sheets Don't Need To Be Updated for OTC Medications
Over-the-counter (OTC) medications can interact with prescription medications and affect a patient's health. Hence, they should also be documented on the MAR sheet. This ensures a comprehensive view of all substances the patient is consuming, allowing for safer and more effective care.
Key takeaways
Filling out a Medication Administration Record Sheet correctly is crucial for ensuring that individuals receive their required medications accurately and on time. This simple act helps in maintaining an organized medication management system, especially in settings where multiple individuals are being cared for. Here are key takeaways to consider when handling this form:
- Always start by filling in the consumer's name, the attending physician's name, along with the month and year. These details are fundamental to ensure the correct handling and administration of medication.
- Record the medication and corresponding administration hours clearly. This schedule forms the backbone of the daily medication plan, and clarity here prevents mistakes.
- Understand and use the special codes accurately: R for Refused, D for Discontinued, H for Home, D (Day Program), and C for Changed. These codes provide critical information about the medication administration process.
- Meticulously record at the time of administration. This habit ensures real-time tracking and minimizes the risk of administering medication twice or not at all.
- In the case where a consumer refuses medication, mark it as 'R' and notify the attending healthcare provider as soon as possible. Such instances need to be addressed immediately to understand the reason behind the refusal.
- When medication is discontinued, clearly mark it with 'D' and remove the medication from the schedule to prevent accidental administration.
- If the consumer is at home ('H') or attending a day program ('D'), note this on the form to explain any deviations from the typical administration schedule.
- Any change ('C') in medication, whether it's in dosage, frequency, or type, must be updated on the sheet as soon as the change is prescribed. Consistency in tracking changes ensures continuity of care and medication accuracy.
- Finally, maintain a clean and organized record. Any errors, cross-outs, or illegible entries can lead to confusion and potential medication errors, the consequences of which could be serious.
Proper use of a Medication Administration Record Sheet not only adheres to good practice standards but also underpins the safety and well-being of the consumer. Therefore, paying close attention to detail and following these key takeaways is essential for anyone responsible for medication administration.
Common PDF Forms
I 9 Documents - An Employment Verification Form is a document used by employers to confirm the employment status of current or former employees.
Printable Cash Count Sheet Excel - Streamlines the cash reconciliation process, saving time and reducing stress for employees and managers.