Free Tb Test PDF Form
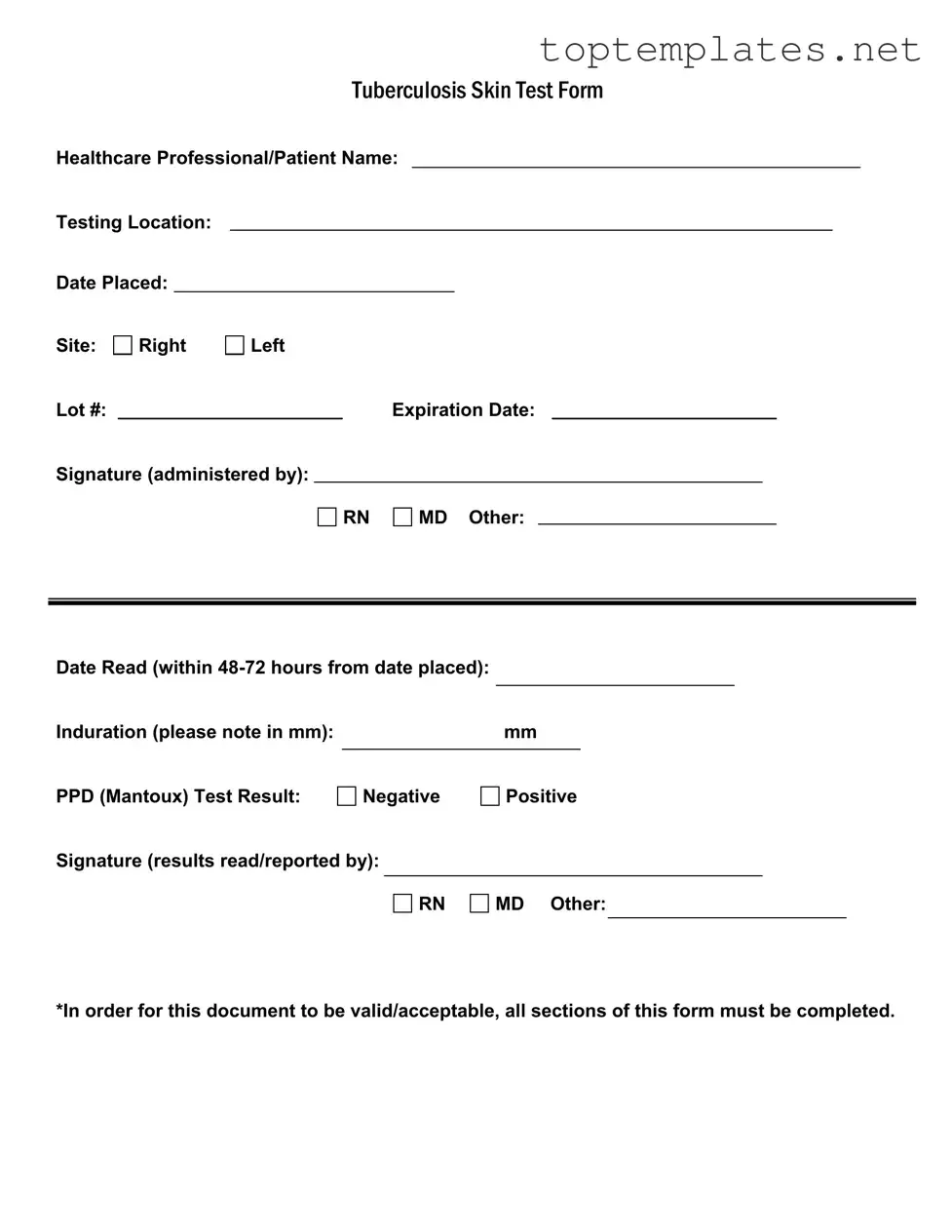
In the landscape of public health and preventive medicine, the Tuberculosis (TB) Skin Test Form plays a crucial role in the early detection and intervention of tuberculosis, a contagious bacterial infection that primarily impacts the lungs but can also affect other parts of the body. This form serves as a standardized template for healthcare professionals to document the administration and reading of the Mantoux Tuberculin Skin Test, a primary method used to identify TB infections. The form captures essential information including the healthcare professional or patient's name, testing location, dates related to the placement and reading of the test, site of the test injection (either right or left arm), lot number and expiration date of the tuberculin used, and the details of the person administering and reading the test, which may include registered nurses, medical doctors, or other qualified healthcare workers. Additionally, it records the test outcome in terms of induration size in millimeters and categorizes the test result as negative or positive. The signatures of the individuals responsible for administering the test and reading the results are indispensable, underscoring the authenticity and integrity of the process. This form not only facilitates efficient communication and record-keeping among healthcare providers but also ensures compliance with public health guidelines, stressing its importance in the grand schema of TB prevention and control strategies. For the document to be considered valid and acceptable, it mandates the completion of all sections, emphasizing the thoroughness required in tracking and managing potential TB cases.
Sample - Tb Test Form
|
|
|
|
|
TUBERCULOSISSKINTESTFORM |
||||||||
Healthcare Professional/Patient Name: |
|||||||||||||
Testing Location: |
|
|
|
|
|
|
|
|
|
|
|
||
Date Placed: |
|
|
|
|
|
|
|
|
|
|
|
|
|
Site: |
Right |
Left |
|
|
|
|
|
|
|
|
|||
Lot #: |
|
|
|
|
|
Expiration Date: |
|
|
|||||
Signature (administered by): |
|
|
|
|
|
|
|
|
|
||||
|
|
|
|
|
RN |
|
MD Other: |
|
|
|
|||
Date Read (within |
|
|
|
|
|
|
|
Induration (please note in mm): |
|
mm |
|
PPD (Mantoux) Test Result: |
|
|
|
Negative |
Positive |
||
Signature (results read/reported by):
RN
MD Other:
*In order for this document to be valid/acceptable, all sections of this form must be completed.
File Specs
| Fact Name | Description |
|---|---|
| Form Content | The TB Test Form includes sections for; Healthcare Professional/Patient Name, Testing Location, Date Placed, Site, Lot #, Expiration Date, and signatures for administration and results. |
| Test Placement Site Options | The form provides options to select either the right or left site for the test placement. |
| Test Reading Window | Results must be read within 48-72 hours from the date the test was placed. |
| Result Interpretation | The form requires the induration size in millimeters (mm) and the PPD (Mantoux) Test Result to be either negative or positive. |
| Professional Qualifications | Signatures are required from licensed professionals (RN, MD, or Other) for both the administration of the test and the reading/reporting of results. |
| Validity Requirement | All sections of the form must be completed for the document to be considered valid/acceptable. |
| Governing Laws | This document is subject to state-specific laws and regulations regarding tuberculosis testing and reporting in the healthcare sector. |
| Administration and Reading Signatures | Two distinct signatures are required on the form; one for who administered the test and another for who read/reported the results. |
| Use in Healthcare | The TB Test Form is widely used in healthcare settings to screen individuals for tuberculosis. |
Steps to Filling Out Tb Test
Completing the TB (Tuberculosis) Test form is a critical step in ensuring the health and safety of individuals, particularly those who work in environments where TB exposure is a concern. This form records the administration and results of a Tuberculosis Skin Test, often required for employment in healthcare settings, educational institutions, and other high-risk areas. To ensure the form is filled out correctly and efficiently, it’s important to follow each step with attention to detail. Accuracy is not only a matter of compliance but also a reflection of commitment to public health.
- Healthcare Professional/Patient Name: Begin by printing the name of the individual undergoing the TB test. Ensure the name is spelled correctly and matches identification documents.
- Testing Location: Record the name or identifier of the place where the test is conducted. This information is crucial for tracking and record-keeping purposes.
- Date Placed: Enter the date when the test was administered. It’s important to use the format MM/DD/YYYY to avoid any confusion.
- Site: Mark whether the injection was placed on the right or left forearm. This detail helps in verifying and interpreting the test results accurately.
- Lot #: Note the lot number of the test administered. This information, found on the test packaging, is essential for tracking the test solutions and ensuring their validity.
- Expiration Date: Write down the expiration date of the test solution used. Using an expired product can lead to inaccurate results.
- Signature (administered by): The healthcare professional who administered the test must sign here, indicating their role as RN, MD, or Other. This signature validates the administration process.
- Date Read (within 48-72 hours from date placed): Enter the date when the test result was read. It’s crucial to read the result within the 48-72 hour window for accurate interpretation.
- Induration (please note in mm): Record the size of the induration (if present) in millimeters. This measurement is critical in determining the test result.
- PPD (Mantoux) Test Result: Indicate the test result as either Negative or Positive. This conclusion is based on the measured induration size and clinical guidelines.
- Signature (results read/reported by): The individual responsible for reading and reporting the test result should sign here, noting their role as RN, MD, or Other. This signature is essential for validating the test outcome.
Upon completing the TB Test form, it is paramount that all sections are reviewed for completeness and accuracy. Missing or incorrect information can lead to delays or the necessity to redo the test, affecting timelines and potentially health outcomes. Following the outlined steps ensures a thorough and compliant documentation process, facilitating a smooth operation for healthcare providers and contributing to effective public health monitoring.
Discover More on Tb Test
What is a TB (Tuberculosis) Skin Test Form?
A TB Skin Test Form is a document used by healthcare professionals to record the details and results of a Tuberculosis (TB) skin test, also known as the PPD (Purified Protein Derivative) Mantoux test. This form includes information such as the healthcare professional or patient's name, the testing location, the date the test was placed, the site of the test (either right or left arm), the lot number of the test, its expiration date, and signatures from the person administering the test and the person reading the results. It's crucial that every section of this form is completed for it to be considered valid.
How is the TB skin test read, and what do the results mean?
The TB skin test is read between 48 to 72 hours after it is administered. The test is evaluated by measuring the induration (swelling) at the site of the injection in millimeters. A healthcare professional will record this measurement on the TB Skin Test Form. A result is considered positive when the induration meets or exceeds a certain size, indicating a TB infection. Negative results indicate that no TB infection was detected. However, the size criteria for a positive result can vary depending on the individual's risk factors and health history.
Who is authorized to administer and read the results of a TB Skin Test?
Qualified healthcare professionals such as Registered Nurses (RNs), Medical Doctors (MDs), or other authorized practitioners can both administer the TB skin test and read the results. The individual who administers the test and the one who reads the results will both sign the TB Skin Test Form to validate the procedure and the findings. It's important for both roles to be performed by professionals who are trained and knowledgeable about the TB skin test procedure to ensure accuracy.
Is it mandatory to complete all sections of the TB Skin Test Form?
Yes, it is essential to fill out every section of the TB Skin Test Form for it to be considered valid and acceptable. This includes all personal information, details about the test administration, and the results section. Incomplete forms may lead to misunderstandings or misinterpretations of the test results and could require the test to be administered again. Ensuring that the form is fully completed helps in maintaining accurate and reliable records of TB skin test results.
Common mistakes
When completing the Tuberculosis (TB) Skin Test Form, individuals often make mistakes that could affect the test's validity. Recognizing and avoiding these errors is crucial for ensuring the form's acceptance and the accuracy of the test results.
Not completing all sections: Every section of the form must be filled out for it to be valid. Omitting information, such as the healthcare professional or patient name, testing location, or signatures, can lead to the form's rejection.
Incorrectly documenting the injection site: The form requires specifying whether the test was administered on the right or left arm. Misidentifying the site can cause confusion in reading the results.
Failing to note the induration size in millimeters: Precise measurement of the induration is critical. Recording this measurement inaccurately or not at all can impair the test result's interpretation.
Misreporting the test date: The test must be read within 48-72 hours after it is placed. Incorrectly noting the dates can invalidate the test due to the precise time window required for accurate results.
Forgetting to include the lot number and expiration date of the test administered: This information is crucial for tracking the test's validity and ensuring it was effective at the time of administration.
Omitting or incorrectly providing signature and designation of the person administering the test and the one reading the results: Signatures validate the test's administration and reading. Failing to properly indicate the person's role (RN, MD, Other) can lead to questions regarding the test's validity.
To ensure the TB Skin Test Form is correctly completed and accepted:
- Review each section carefully before submission.
- Double-check measurements and specific details such as induration size and test dates.
- Ensure that both the individual administering and reading the test clearly sign and indicate their professional designation.
By avoiding these common mistakes, the integrity of the TB test process is upheld, contributing to accurate and reliable health assessments.
Documents used along the form
When a Tuberculosis (TB) Skin Test is administered, several other forms and documents may be required to ensure comprehensive healthcare management and to comply with legal or organizational requirements. These documents help in tracking the patient's health status, ensuring proper treatment protocols are followed, and maintaining a complete health record.
- Vaccination Record: This document keeps track of all vaccinations a person has received. It's particularly important in the context of TB testing to identify if the BCG vaccine (which can influence TB test results) has been administered.
- Health Screen Consent Form: Before conducting a TB test, or any other health screening, consent must be obtained from the patient. This document ensures that the patient understands the procedure and any associated risks.
- Employment Health Screening Form: Often used in occupational health, this form assesses an employee's suitability for a job role, based on their health status. It may include TB test results among other health metrics.
- Immunization Exemption Form: For individuals who cannot receive certain immunizations due to medical, religious, or personal reasons, this document formally records their exemption status.
- Medical History Form: This comprehensive form records a patient’s medical history, including past illnesses, surgeries, and treatments which could affect the interpretation of the TB test results.
- Exposure Incident Report: If the TB test is part of post-exposure management, this document records details of the exposure incident, including the type of exposure and any immediate measures taken.
- Symptom Checklist: This form can be used to document any symptoms the patient may be experiencing that are relevant to TB or another ailment, aiding in diagnosis and care planning.
- Treatment Consent Form: If a TB test comes back positive, and treatment is necessary, this document outlines the treatment plan and secures the patient's consent to proceed.
- Follow-up Appointment Schedule: This document helps manage and track the patient’s follow-up appointments, which are essential for monitoring treatment progress or assessing any change in condition.
Adequate documentation, including the TB Test Form and the associated documents listed above, plays a crucial role in patient care and legal compliance in medical settings. Ensuring that all relevant forms are accurately completed and properly maintained supports effective healthcare delivery and patient safety.
Similar forms
Vaccination Record Card: Similar to the TB Test Form, a Vaccination Record Card documents important health-related events, in this case, vaccinations received by an individual. Both forms record dates, healthcare professional information, and signatures for verification. Their primary function is to track and provide evidence of health interventions, ensuring that individuals have received necessary treatments or tests for public health and personal wellness.
Medical Prescription Form: This document shares the TB Test Form's structure in capturing healthcare professional details, patient information, and specific medical interventions. Prescriptions specify the medication, dosage, and administration instructions, akin to how the TB Test Form details the test type, site, and result. Each form relies on the healthcare provider's signature for authenticity, crucial for the subsequent action—be it drug dispensation or interpreting medical test outcomes.
Consent Form for Medical Procedures: Consent forms are integral to the medical field, documenting a patient's agreement to undergo a specific procedure or treatment. Like the TB Test Form, consent forms include identifying information, details of the procedure (including risks and benefits), and signatures from both the patient and healthcare provider. The parallel lies in their mutual requirement for informed acknowledgment by both parties before proceeding with a healthcare intervention.
Laboratory Test Order Form: This form serves a similar purpose by specifying tests ordered by a healthcare provider, mirroring the TB Test Form's function of outlining a specific diagnostic test. It typically includes patient information, test details, and instructions for the laboratory, ensuring that the correct tests are performed. Both forms play a pivotal role in the diagnostic process, guiding healthcare professionals in making informed decisions about patient care.
Health Screening Form: Health screening forms are used to record the outcomes of various health assessments, akin to how the TB Test Form documents the result of a tuberculosis skin test. They include personal and healthcare provider information, testing details, and the screening outcomes. By capturing this information, health screening forms, much like the TB Test Form, assist in monitoring and maintaining public and individual health standards.
Dos and Don'ts
When it comes to completing the TB Test form, accuracy and thoroughness are key. Here's a straightforward list of things you should and shouldn't do to ensure the process goes smoothly:
Do:- Verify all information before submitting the form. Make sure names, dates, and other details are correct and match any accompanying identification or records.
- Ensure the testing location is accurately listed. This can help in the event of any follow-up or verification needed.
- Use the correct format for dates, typically MM/DD/YYYY in the U.S., to prevent any confusion.
- Have the signature of the professional who administered the test included. Whether it's an RN, MD, or other, their endorsement is crucial for the form's validity.
- Mark the site of the test (right or left arm) clearly. This can be important for tracking reactions or if retesting is required.
- Leave any sections incomplete. Each part of the form needs to be filled out to ensure its acceptance and validity.
- Guess on specifics, like lot numbers or expiration dates. Incorrect information can invalidate the test result or lead to administrative issues.
- Delay the reading of the results beyond the recommended 48-72 hours after the test is placed. Timing is essential for accurate interpretation of the test.
- Forget to include the signature of the person who interpreted the test results. Just like the administrator's signature, this is necessary for the form to be complete.
By following these guidelines, you can help ensure that your TB Test form is correctly filled out and accepted without any problems. Remember, taking the time to double-check details now can save a lot of time and hassle later.
Misconceptions
There are several misconceptions surrounding the Tuberculosis (TB) Skin Test Form, which may lead to misunderstandings about its administration and interpretation. Below are five common misconceptions and clarifications to help dispel these errors.
- Misconception 1: A positive skin test always means you have tuberculosis.
This is not accurate. A positive TB skin test indicates that the person has been infected with the TB bacteria, but it doesn't necessarily mean active tuberculosis disease is present. Further examinations, such as a chest X-ray and sputum tests, are required to confirm whether the infection is latent or has progressed to active disease.
- Misconception 2: Only an MD can administer and read the results of a TB skin test.
The form clearly provides options for an RN or 'Other' healthcare professionals to both place the test and read the results. This indicates a broader range of qualified healthcare workers can be involved in this process, not solely MDs.
- Misconception 3: The TB skin test is the only screening tool for tuberculosis.
While the Mantoux tuberculin skin test (PPD test) has been a longstanding method for detecting TB infection, it's not the only screening tool. There are blood tests known as interferon-gamma release assays (IGRAs) that sometimes are recommended over the skin test in certain cases.
- Misconception 4: The test site must always be on the left arm.
The form specifies that the injection site for the TB test can be administered on either the right or left arm, debunking the myth that it must always be done on the left. This choice allows healthcare professionals to choose the best site for injection based on individual patient considerations.
- Misconception 5: If you forget the initial reading, it’s fine as long as you get it done eventually.
The requirement for reading the results within 48-72 hours from when the test was placed is critical for accurate interpretation. Delays beyond this window can lead to inaccurate readings, which may necessitate retesting for reliable results.
Understanding these aspects of the TB Skin Test Form is crucial not only for healthcare professionals but also for individuals undergoing testing. It ensures a clear comprehension of the procedure and interpretation of results, guiding appropriate next steps in care and treatment.
Key takeaways
Understanding the Tuberculosis (TB) Skin Test Form is crucial for healthcare professionals and patients alike. The form, simple yet significant, ensures the proper administration and interpretation of the TB skin test. Here are nine key takeaways that everyone should keep in mind:
- Complete all sections: For the form to be considered valid, every section must be filled out. This ensures that all relevant details about the test, including administration and results, are fully documented.
- Healthcare Professional/Patient Name: Clearly identifying both the healthcare professional and the patient is essential for accurate record-keeping and follow-up.
- Testing Location: Recording where the test is conducted helps in maintaining a clear record, should there be a need to trace the testing environment or conditions.
- Date Placed: The date when the TB skin test is administered is critical, as the reading must occur within a specific timeframe to ensure accuracy.
- Site: Indicating whether the test was placed on the right or left forearm is important for consistency in testing, particularly if repeat tests are necessary.
- Lot # and Expiration Date: Documenting the lot number and expiration date of the test material is crucial for quality control and in case of any recalls or issues with the test batch.
- Signature of administrator: The signature of the person who administered the test adds a layer of accountability and ensures that a qualified professional has conducted the procedure.
- Date Read: The test must be read within 48-72 hours after administration. Recording the exact date and time of reading is essential for validating the results.
- Results recording: The form should clearly indicate the induration measurement in millimeters and whether the test result is negative or positive. The signature of the person reading and interpreting the result is also necessary for verification purposes.
Accurately completing the TB skin test form is a vital step in TB management and control. By adhering to these guidelines, healthcare providers can ensure that each test is administered and interpreted correctly, thereby safeguarding patient health and contributing to public health efforts against tuberculosis.
Common PDF Forms
Dd 214 - Features the social security number for identification within military records.
Phone Insurance Claim - The form directly impacts customer satisfaction by minimizing confusion and clarifying what information is needed and why it is important.
Evaluation Basketball - Its focus on both individual skills and team-oriented abilities ensures that player evaluations are comprehensive and conducive to team strategy.